Before The Truth Can Get Its Boots On

This essay is brought about by a story that keeps being mistold. As stories go, it is rather an old one. It is about a medical scandal and people with M.E.
I say people, but the majority of those who have Myalgic Encephalomyelitis are women. Many of us were just girls when we became ill.
The symptoms are wide-ranging and vary from person to person. Common symptoms include debilitating exhaustion, pain, flu-like symptoms, sensitivity to sound and/or light, memory problems, burning pain and orthostatic intolerance (dizziness when you stand). The defining symptom is something called post-exertional malaise which is just a fancy way of saying that when you do a normal activity it makes you ill and you don’t recover from it quickly.
In the severely affected this might mean that it takes days, or longer, to recover from something as simple as standing up or walking a few steps. Or, that an attempt at a slightly more robust task sees you bedbound for weeks or months. In comparatively less affected people it might mean that after the lovely cup of tea you’ve had with a friend at a café, or after working at your morning part time job, you then have to spend time back in bed having to do nothing and waiting for your body to catch up with you before you can try again. You can’t replenish expended energy like a normal person.
In the especially bad cases, it may mean that having reached the stage of illness where you are bedbound, it is then years before you can do much of anything at all. If ever again.
For many years my primary cause, along with friends, was to raise awareness of the illness and to help raise funds for biomedical research into it. With little to no medical help, while suddenly being greatly unwell, sufferers are having to collectively fathom their way out of the situation they find themselves in.
We are all Poirots with rebellious little grey cells that keep forgetting things, as we try to research answers.
There is a remarkable amount of joy, resilience and creativity to be found among M.E patients. I have known friends to paint pictures, painstakingly, a few strokes a day and others who write, just as laboriously, but make beautiful stories out of that patience. We are a community of people who have to wait like the tide, to wash the rock to sand in our own time.
You may not forgive me, but I was one of the poets. I suppose I still am but the discussion of issues around women’s rights and gender rather derails these things. Long before I made it onto the internet, or could even write them down, my poems kept me company and my stories meant I could escape what was happening to me, at least for a little.
My early online poems were small things but being able to share them wrote me into the world a little more. Amazingly, no one ever pelted me with tomatoes and begged me to stop. (They haven’t lost their chance).
In the early, early days before the internet we kept in touch via letters. If you were young enough there was a children’s charity, called AYME, who put you in touch with others going through the same. I was, and I had a habit of going through the list of new members, finding names I particularly loved and sending a friendly letter to them through the charity head office. Often, I had to dictate them to my mum. If they were too sick to write back, their mothers usually wrote back for them, too.
Many of my teenage peers in the charity back then had been ill since they were six, or seven, or eight years old. I was an oldie, having only developed M.E at the grand age of twelve. I still remember the heart stopping feeling of seeing a little girl called Eden in the membership list, aged five. I didn’t write to her but I thought about her when I couldn’t climb the stairs, or the pain gathered in, in ways I couldn’t comprehend happening to an even younger child.
While there is sadness in such communities, there is more laughter. The shared suffering is a bond, but on top of that you have hijinks and stories and all manner of daydreams. You tell each other that you will all get better, and paint the town a thousand colours, and dance with Princes or film stars, and chase careers and really make something out of life.
You learn how to make something out of the life you are living, too. Even though it is one with higher walls and closer parameters than most people can comprehend.
The worst sadness in these communities is usually when people die. Something that I didn’t start experiencing until my peers and I were adults. People can die of M.E, though it is rare. One of my youngest friends with M.E lost her life to the illness at the age of twenty-one. Her smile when it came, even in those last years, could’ve lit the beacons.
Others die with it instead, but in my experience they die younger than might be expected. Perhaps it just wears us out. Some patients also take their own lives. I imagine healthy people see that as a sign of depression or fragility. I know that it is simply because extraordinary pain is sometimes too much for someone. Particularly with an illness that medicine is largely unable to mitigate.
More than that, M.E sufferers have often been treated as some version of contemptible. For example, one leading gastroenterologist, at the Mayo Clinic, is on record saying: “The average doctor will see they are neurotic and he will often be disgusted with them”.
Callous as he may be, he did not conjure this version of us from his own imagination. He has instead borrowed from certain doctors who came before him.
MIXED BEGINNINGS
It’s hard to trace the entire history of M.E but it is likely that it has existed for centuries, with some doctors pointing to potential outbreaks as far back as the late 1600s1
It wasn’t until an article in The Lancet in 1956, that it got a permanent name. The authors write, “It remains to identify this syndrome more precisely; but we believe that its characteristics are now sufficiently clear to differentiate it from poliomyelitis, epidemic myalgia, glandular fever, the forms of epidemic encephalitis already described, and, need it be said, hysteria.”2
It still needs to be said.
Unfortunately, saying it back then made little difference to what, ultimately, happened. One of the discussion points of that Lancet article was various outbreaks over the years. The Royal Free Hospital outbreak, of the year before, was mentioned. That outbreak is a touchstone of M.E history most patients will have heard of because it ended up informing how much of the medical profession chose to approach the disease. For a short time the condition was even known as “Royal Free Disease”.
In 1955, from July to November, 292 members of the medical and administrative staff working at the Royal Free Hospital, in London, were struck down by a mysterious illness. Of those, at least 255 were admitted to hospital.
According to an M.E Association overviews of events3
“It made newspaper headlines. It baffled doctors. Its wide-ranging symptoms – muscle weakness and pain, extreme tiredness, headache, even vertigo – left them scratching their heads. Some suspected it was polio-type illness. But all blood tests came back negative.
Science – medicine – drew a blank. But no-one disputed that what the patients had suffered was a real and physical illness, bringing misery riding on its coattails. Some patients recovered, but many would never feel well – never work again.”
Enter McEvedy and Beard, two male psychiatrists, during the flared trouser heights of 1970. They published a paper, “Royal Free Epidemic of 1955: A Reconsideration” ,which did what it said on the tin and reconsidered the events in order to suggest hysteria was really the cause. They managed to conclude this despite not speaking to anyone who had actually been present at the time. A bit of a desk and sandwich job4
Their first listed reason for their conclusion is telling, “the high attack rate in females compared with males”.
The smoking gun, apparently, is the female sex.
It is hard to overstate how influential this paper was for a generation of doctors. More recently, a 2021 re-examination (Underhill & Baillod) of McEvedy and Beard’s paper has refuted their conclusions. It notes:
“Research studies in patients with ME/CFS have shown multiple pathophysiological differences between patients and healthy controls in the immune system, the nervous system, and metabolic processes including energy metabolism. Although no causal pathogen has been identified, studies have shown that patients harbor a variety of infectious agents and have pointed towards a possible aetiological role for infectious organisms. The psychosomatic hypothesis does not explain these pathophysiological changes. Mathematical modeling of the Royal Free outbreak also validates an infectious disease aetiology and refutes the epidemic hysteria hypothesis”5
Good quality research into M.E, when and where it is done, is riveting. Far from being unable to find much wrong with us, it seems we have been holding ourselves together with silly string and creaking hinges all these years. Doctors are looking at everything from our blood6 (behaving badly) to our energy cells7 (behaving badly) to our brain8 (apparently inflamed). Still, this remains an area of medicine much overlooked and dismissed because of the efforts of certain segments of psychiatry.
In the aforementioned 2021 re-examination of McEvedy and Beard’s paper the authors did what those two hadn’t done and got first hand accounts from people who had been there. Both from those who did, and did not, develop the illness.
They concluded, “Based on the recollections of all the 27 ex-Royal Free hospital staff and medical students who provided data for this study, hysteria as the underlying cause of the Royal Free outbreak seems inconceivable”.
Another argument McEvedy and Beard had put forward for their assertion of hysteria was the suggestion that a lot of patients experienced “overbreathing”, more commonly known as hyperventilation. Something that has been reported to be present in up to a third of mass hysteria outbreaks, as well as present in 40% of schoolgirls in a specific form of mass hysteria that McEvedy and Beard referenced when talking about Royal Free patients. They speculated that those at Royal Free were, “a frightened and hysterical population whose over-breathing was intermittent and covert”. It is a puzzle to imagine why they thought well-trained hospital and medical staff, who are used to dealing with medical emergencies, could be described in such a way.
A raised respiratory rate was only present in four, severely ill, patients and no overt hyperventilation was reported either at the time, or later, by those who had been there.
Another key distinguishing feature between the Royal Free Outbreak and hysteria was gestation time. Hysteria rather sweeps about the place gathering victims as it goes. It can generate between people quickly. Rather like panic tends to do. It is a pied piper, not an accountant. So, it does not make an appointment with you in advance and wait patiently for you to get around to stopping by. Yet, the incubation period for patients at Royal Free was several days.
When you separate people with hysteria, or remove them from the environment the hysteria is happening in, they tend to perk up a bit. Not so, with those sent home during the Royal Free outbreak who continued to be ill.
To me, it is clear that medical sexism met science and somehow won when the McEvedy and Beard paper gained such ridiculous traction and cast M.E patients as hysterical.
The consequence of this for patients is impossible to quantify. Those with the illness have been denigrated and dismissed. So many have lost decades to an illness that was never properly researched or investigated because we were considered to be hysterical. Millions of people have had to face this illness without hope of cure or treatment. This has meant it has necessarily been more serious than it otherwise might be.
Unfortunately, it is often serious. Approximately 25% of patients with M.E are bed bound or housebound. Often for decades.
A recent Danish study found patients' quality of life scores were, “significantly lower than the population mean and the lowest of all the compared conditions.”. Compared conditions included lung cancer, diabetes, long term mental illness, osteoarthritis, heart attack and stroke9
The authors state, “The condition can be as disabling as multiple sclerosis, rheumatoid arthritis, systemic lupus erythematosus and congestive heart failure” and called for further research to confirm their own findings.
This builds on clinical knowledge and on previous studies, from several countries, which found similar grim results for this patient group when comparing patient quality of life to other conditions.
I doubt we can measure the toll on parents whose children with M.E were taken away from them by authorities, either. Or who were threatened with that and had it hanging over them while they were trying to care for their child. All because certain doctors were sure the children weren’t really physically sick and thus the parents must be the issue. My own parents heard of cases like this and worried about what might happen and how they would protect me. Especially after it happened to one of my pen friends10
So many patients have struggled hand-to-mouth for years because they could not work and there was not much help for them. There was not much help because they were derided as malingerers.
Despite their troubles, and an environment in which the media and medical profession have treated those who have the disease with scorn, I have rarely found more compassion than from this group of human beings.
It is not a coincidence that, when 75-85% of sufferers are female, such a set of obvious untruths has continued to be told about our patient population. What of the toll, too, on the (most often) young women forcibly removed from their homes and institutionalised on the say-so of doctors11
Such medical missteps have proved either catastrophic by inducing terrible worsenings of the illness or, in the case of U.K. woman Sophia Mirza, they have proved fatal. Sophia decided she didn’t want to go for ‘treatment’ at a specific clinic. She didn’t want to go because such an effort would have made her more ill and for no good reason; her mother had done some research and found out that most patients did not benefit long term from the interventions of the clinic in question.
Patients there were being given graded exercise, and psychological interventions, which are not useful for the disease. Indeed, Graded Exercise Therapy, especially, can make it much worse. In response to making the rational decision to say “no” Sophia was ultimately sectioned under the mental health act and removed from her home.
Criona Mirza writes movingly about her daughter here.
The history of the treatment of M.E patients, I believe, can be distilled down to the brutal sound it must have made when the police broke down Sophia’s door to take her away from those who loved her. A move that was against her interests, her humanity and, ultimately, her life.
This is all the terrible consequence of the fact that after McEvedy and Beard there were plenty of other doctors who kept the momentum of such ideas going. Or reworked the same basic idea as their own.
In America, things were scarcely better. If you want to know how they were tackling this you might wish to read “The Why” by Hillary Johnson. A 92 page polemic on the topic. She is also author of the renowned “Osler’s Web”, which offers greater detail.
MORE RECENT DEBACLES
As many a Victorian wife before us, it has been important to paint M.E patients as sufficiently mad, in order for them to remain within the remit of the asylum. In our case within the remit of psychiatry as a whole. Knighthoods, research projects and whole careers have depended on continuing to portray M.E patients this way and to keep those coffers coming in. After all, if you look in the wrong place for a cure, you can keep looking forever.
Professor Simon Wessely and his acolytes must now enter stage left as the most prominent figures on the scene in the UK, for several decades. Colloquially known as the “Wessely School”, they are an extremely influential group of psychiatrists and certain other interested parties.
The Countess of Mar has spoken eloquently about the influence of the Wessely School in the House of Lords saying that Wessely, “has repeatedly and persistently played down, dismissed, trivialised or ignored most of the significant international biomedical evidence of organic pathology found in ME because it does not fit his psychiatric model of the disorder”12
Adding that the Wessely School believes that “it should be classified as a mental disorder over which they should exert control.”
This runs contrary to the World Health Organisation’s position on the illness as they do not, and have never, classified it as a psychiatric disorder.
She adds that the group, “has gained dominance in the thinking about ME/CFS. Wessely is politically astute and, in conjunction with his colleagues, has gained respectability in medical and political establishments by producing vast numbers of papers that purport to be about ME”.
The treatments the Wessely School continually push for are Cognitive Behavioural Therapy and Graded Exercise Therapy. She raises an important ethical conflict of interest Wessely has had here, “Among his 53, largely undeclared, interests it should be noted that he is a member of the supervisory board of a company, PRISMA, that is supplying such rehabilitation programmes as CBT to the NHS for those with ME”.
She tells us that one of the recurring themes in his papers, besides the insistence M.E is a psychiatric illness, is the belief that one of the factors to play an important role in the perpetuation of the disorder is being female. Not because of our biology, you understand; It is our psychology he imagines to be important.
She quotes him, too, talking about patients. He says M.E sufferers, “feel no guilt about their condition…”, and that the illness, “should not be dignified by [its] own formal case definition and body of research". Going so far as to suggest that the “muscle weakness is simulated".
The Wessely School, she states, have also actively “stifled access to research funding for any UK researchers who want to consider organic causes of the disorder.”
Another well known woman taking up the torch for sufferers is Margaret Williams. She has M.E, herself, and worked in the NHS in a senior clinical capacity until M.E ended her career. In one 2003 document, she highlighted more Wessely School conflicts of interest via certain members' involvement with insurance companies. This included international efforts to help insurance companies deny claimants with M.E. One of the companies in question was UNUM, a leading U.K. employee benefits provider. UNUM was additionally “advising the UK Benefits Agency doctors on how to deal with chronically ill ME patients”13. See also Hooper14
Margaret wrote a thirty year retrospective of Wessely’s own career which demonstrates the British art of initially seeming to praise someone while actually eviscerating their incredible failures.15
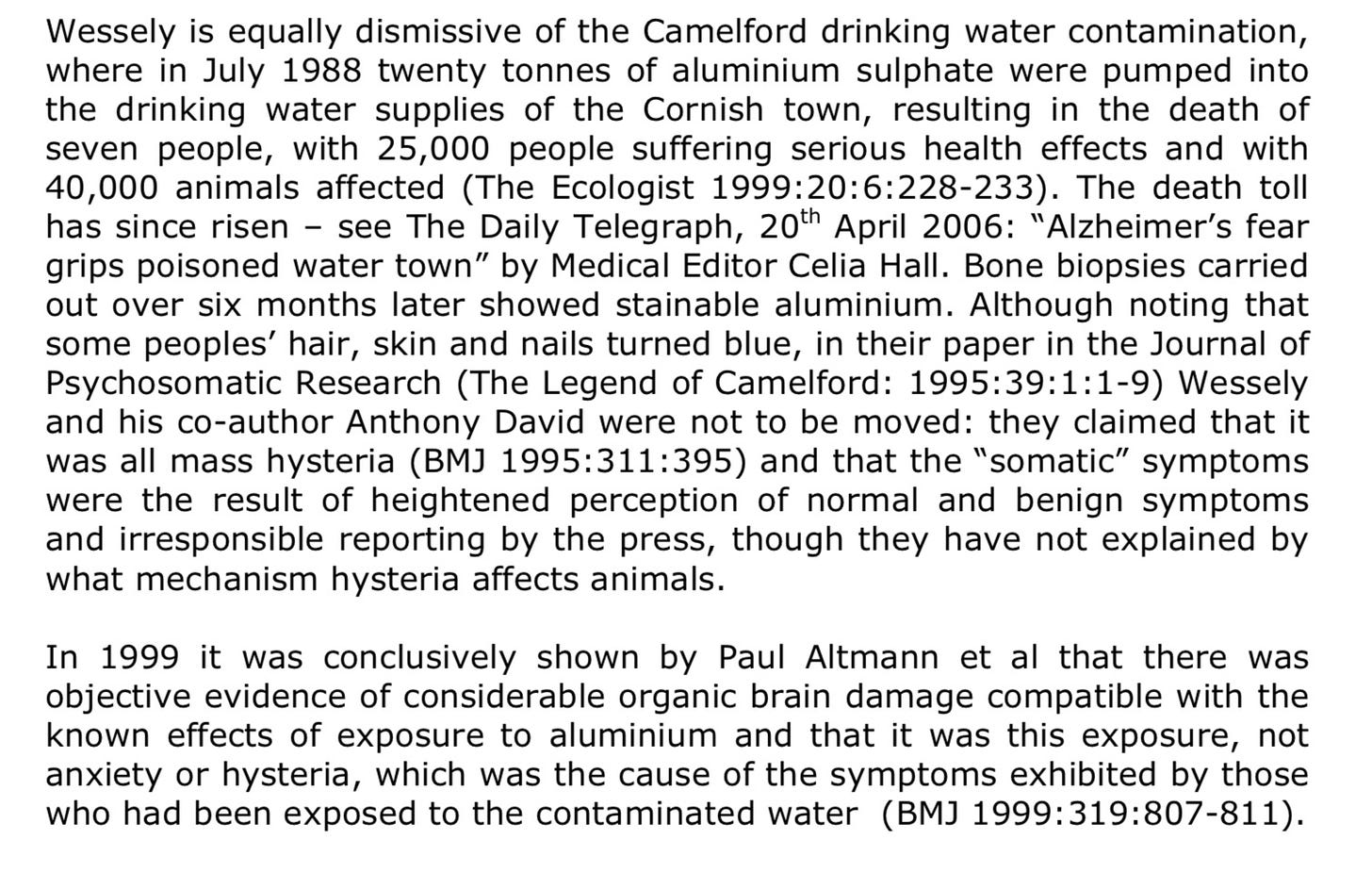
One of which was his assertion that victims of the Camelford Water Poisoning, Britain’s worst water poisoning event, were suffering from mass hysteria.
To wit (Hooper & Williams)16 :
Of course, we can scarcely blame him for holding the highly scientific belief that hysterical people can turn their hair, skin and nails blue at will.
You really can’t keep the good doctor down though. The list of his honours is almost as large as the list of harms he has left in his wake.
His ideas seem to have the worrying ability to be able to persist long after they have been disproven, too.
Wessely was one of the architects of the cognitive behavioural model for M.E, proponents of which like to talk about patients “irrational illness beliefs” and their “fearful cognitions”. These are supposed to be making sufferers ill. The very act of a patient attributing their illness to a physical cause is used against them as proof of their irrationality.
A 2019 review conducted by Geraghty et al, examined the cognitive behavioural model to see how good a fit it really was for M.E. Wessely is even quoted here admitting the evidence for the model he has so fervently pushed is weak. That, of course, hasn’t stopped him.17
Examples of the method scarcely make it look scientific “The CBM aims to change patients’ unhelpful thoughts and experiences of symptoms (pain, fatigue and malaise) with supplanted alternatives. ‘I am sick, I think its related to an infection, I am tired’ (patient) to ‘you do not have an organic disease, resting is harmful, you can do activities’ (CBT therapist).”
I can imagine that last quote being said by a capitalistic robot in a science fiction story as he pushes people with the flu out the door to go work down the lithium battery mines. Just me?!
Another thing proponents of this model believe is that M.E patients are sick because of “the rewards of the sick-role, social care benefits and peer support in sickness (Halligan and Aylward, 2006). The assertion is made that a return to normal activity would result in the loss of such social benefits and that ME/CFS sufferers remain sick to avail sick-role benefits”.
Perhaps to someone who hasn’t experienced M.E that speculation sounds less contemptible than it is.
Many people with it are stuck in darkened rooms, wearing earplugs because their senses hurt them. They are bedbound and isolated. They are in great pain. Their limbs feel so heavy that any movement requires Herculean effort, if it can be achieved at all.
When I was at that stage I had to be left entirely on my own except for the few moments a day I was brought food. There are many M.E patients who spend more years in solitary confinement than a murderer.
At that time, I could not physically speak and it was excruciating to listen. Touch hurt me so no one could sit beside my bed to hold my hand.
Letters from my friends (both ill and well friends) gathered in the dining room because I was unable to read them or have them read out to me. Text messages from loved ones, like my darling Grandpa, went unread for years on my turned off phone. By the time I was well enough to have turned it back on again he was long dead.
As is the case for so many others, I wasn’t well enough to be online back then, I could not read or write or watch television. Occasionally, wonderfully, I could manage the radio on very low for a half an hour episode of something on the BBC. Occasionally, wonderfully, I could read a paragraph and cherish it for weeks.
You face severe M.E alone. You live behind your closed eyelids and you endure. If you are very lucky, it lets you go enough for you to be able to talk about those parts of it in the past tense.
What peer support, what social benefit do they imagine? What sick role benefits do they foresee? Even for less ill patients, are we really meant to think they value other people’s supposed pity and sorrow over their freedom to do what they want to do?
Perhaps such people exist. Still, they’d have to be a special kind of absurd to pick as their manufactured illness one that has been so maligned in the press, and is routinely denigrated by members of the general public as a result. Not to mention an illness that sees swathes of the medical profession treat you as so much unfortunate gum beneath their proverbial shoe. The stigma against M.E sufferers is widespread.
I cite the most telling part of the conclusion to the Cognitive Behavioural Model review which explains how tinpot this model is for our patient group “This model is often cited in the literature as a model to guide clinical practice and treatment of this illness. We find this model to be primarily an idealised narrative model. It exists as a dogmatic model favoured by model promoters. Our review exposes stark weaknesses, inconsistencies and contradictions, both in its theoretical underpinnings and the research said to prove model validity. Our findings suggest the CBM is not fit for purpose…”
GORGONS AND PACE
There are a lot more politics and individual tragedies I could talk to you about.
There has been a vast amount of money spent on ‘research’ that could never have helped us and a vast amount of money has been denied to research that might have done.
Just as with gender politics, M.E politics can keep you talking indefinitely and saying “and another thing” but for the purposes of giving just an outline of all this let’s turn our attention to the recent U.K PACE trial, and how M.E patients became cultural monsters.
Perceptions of M.E sufferers have often ‘leaked’ into the media from the very people in the medical profession most invested in caricaturing us.
The moniker “Yuppie flu” was popularised by the media at one point, too, and further added to the idea we are all achingly middle class and fey. Clearly only some of us are that 👀. A lower income is, actually, one of the things that translates to a higher risk factor for M.E. While known risk factors for severe M.E are a family history of neurological illness (such as Parkinson’s) and a younger age of disease onset.
The ‘leaking’ of inaccurate perceptions intensified in the wake of the PACE trial. This five million pound trial was conducted by associates of Professor Wessely, running from 2005-2010, and purported to show Cognitive Behavioural Therapy and Graded Exercise Therapy were effective treatments. Wessely himself, “provided feedback on their report”.
These two treatments had already been pushed on patients for many years, without an evidence base, and despite many patients reporting relapse after being trained to dismiss their symptoms and/or attempt to exercise their way out of them.
PACE was partly funded by the Department of Work and Pensions who, perhaps, cherished the hope that a large group of chronically ill patients would need the more inexpensive answers of changing their thinking, and exercise, over the more tangible kinds of support their department exists to offer.
The trial found, unsurprisingly given the beliefs of its authors, that CBT and GET were highly effective.
Jaunty headlines proclaimed, as a result, that patients should “push their limits” and, “Chronic Fatigue Sufferers can overcome symptoms of M.E with positive thinking and exercise”.
The size of the trial (641 patients) meant it had a substantial impact and further seemed to justify the NICE guidelines for patient care which recommended Cognitive Behavioural Therapy and Graded Exercise Therapy, at that time (thankfully no longer). It also directly informed the CDC’s clinical guidelines in America.
As you can imagine there was a lot of disquiet over this in patient communities. Not so much because we disliked the results, although we did, but because we strongly suspected bad science. This concern wasn’t allayed when there was such hesitation from the authors about releasing trial data. What, one wondered, did they have to hide?
The rather protracted, and difficult, battle to find out involved some doctors who have long been supportive of M.E patients. It was rather lovely having them go to bat for us. It also involved patients making Freedom Of Information (FOI) requests, writing letters and asking questions. Something that was later, dishonestly, reframed as harassment of the researchers.
It turned out they had quite a few things to hide such as changing the trial’s protocol midway through. Most eyebrow raising, perhaps, was the decision to introduce post-hoc "normal ranges" for fatigue and physical function.
These ranges were soundly criticised, once they were known, because the thresholds were so low that patients could worsen after trial entry and yet still be considered within the “normal” ranges at the end. This was then used as evidence of their recovery.
Additionally, the study used the Oxford Criteria for M.E which gives a much looser criteria for diagnosis, requiring only six months of disabling fatigue (a symptom that can have many causes). The Oxford Criteria was designed in 1991 by several Wessely School alumni, including PACE author Michael Sharpe. This criteria inevitably leads to a less distinct group of patients, many of whom might not really qualify for an M.E diagnosis at all.
In fact, PACE authors admitted that only 56% of trial participants qualified for such a diagnosis under the, generally, more respected London Criteria. Even here they played fast and loose by using a version of the London Criteria they had modified themselves.
Despite this meddling, later analysis suggests that trial participants who met the altered London Criteria did not fare well and “in up to 82.2% and 79.8% of ME patients their health might have been negatively affected by CBT and GET, respectively.” Even in the whole cohort, which includes those who only met the Oxford Criteria, the number of objective improvers was vanishingly small.18
For several years these crucial pieces of information were occluded and, while the data was withheld, proponents of its unfounded conclusions pushed the idea that the trial was some kind of gold standard of research. This means an unrecorded number of M.E patients will have been subjected to treatments that made them iller as a direct result of PACE. Adding to the numbers of us previously harmed by exercise therapies before PACE was undertaken and published.
Back in November 2015, an open letter was sent to the medical journal, The Lancet, about PACE by six experts in M.E, calling for the trial data to be independently reanalysed. They received no response and wrote several times more, the last letter receiving over 94 signatories. There was no direct response to this, from either the Editor Richard Horton or The Lancet itself.19
Still, the wobbly wheels of the PACE trial were beginning to come off.
The British Medical Journal reported that “Pressure grows on Lancet to review “flawed” PACE trial”. 20
While SAGE later wrote “there is little alternative but to conclude that the PACE team utilised methods that showed CBT and GET to be vastly more beneficial than would have been the case, if the authors used their original trial protocol. The impact of this troubling conclusion is made far worse by the fact that the PACE-Trial authors did not disclose these findings until after the information tribunal”.21
Out of the argy bargy around this trial, and while the hullabaloo was ongoing, a legend emerged. It suggested that M.E patients were akin to terrorists. Newspaper articles verily screamed their headlines; the death threats sent, the researchers harassed, the impossibility of working in the field of M.E research.
How it was easier “to criticise the Prophet Muhammed” than to speak purported truth to the power that is the perpetually napping.
Professor Wessely, leading the rumour mill with great aplomb, added that he had felt safer in the actual war zones of Afghanistan and Iraq than in Britain. Terrible news for the armed forces given he believes that Gulf War Syndrome is another thing people only have because they believe they do.
A cynic might think that diverting attention away from shoddy science towards unverified reports of patient militancy might have been a gambit. Especially as it was the authors of the PACE trial, and their supporters, allegedly getting these threats.
The newspapers seemed more credulous. Yet, reading the articles there’s no concrete evidence that many of us were popping on the war paint, putting a bandana around our heads and mailing expressive death threats to doctors.
Though I would unequivocally condemn anyone who had threatened harm to these doctors, it seems mostly to be high drama and intrigue.
Michael Hanlon, for The Times, informed us that there was a list, somewhere, of 50-80 radical U.K. ME activists. Assuming, for the sake of argument that these people genuinely exist then they would constitute 0.032% of U.K. M.E patients. If they even have M.E at all.
No one reporting on it seemed to be trying to verify either the definite existence of these threats or who sent them if they did exist. There were, instead, some exceptional claims made by a very particular set of researchers being published as fact.
Even the occasional instances that were more clearly relayed by these doctors suggested that, if there was truth in what they were saying, the abuse might be coming to them from men. They had no qualms about selling to the world, through eye-catching headlines, the idea that patients with a disease largely experienced by women were engaged in some kind of guerilla warfare against professionals.
Michael Hanlon told us that Simon Wessely had been facing, “a sustained terror campaign of ME activism”.
So dangerous were the duvet dwellers our hero was up against that a specialised unit at the Metropolitan Police had supposedly been established and dedicated to monitoring the threat.
“No one at Scotland Yard will speak publicly about this” , Hanlon wrote breathily.
“Probably” , as David Black said in Scottish Legal News, “because no such ‘specialised unit’ existed.”
Ironically, it is M.E advocates who have the most noticeable history of trying to find evidence of these kinds of claims. This is the case both here, and in America, where similar claims have been made about patients by clinicians with similar vested interests.
One writer discusses a story about a single crank phone call gaining legs and turning into a story of multiple threats and harassment. Others believe there may be kernels of truth in the claim doctors have received threats but agree there has also been a great deal of exaggeration.22
No evidence has been found of anyone with M.E being charged by the police or convicted in the U.K. courts for harassing or threatening these doctors.
More revealing even than that is documentation obtained under the Freedom of Information Act here from behind the scenes meetings, in 2013. These meetings were attended by some of PACE’s principal investigators. Wessely was also there.23
They discussed the harassment researchers had received and said “harassment is most damaging in the form of vexatious Freedom of Information requests” and noted that “complaints are also causing problems. Researchers are still dealing with complaints about them to the GMC.”
This is a very different picture to the one pushed to the general public. Instead of death threats, their biggest concern amounted to people asking for information and submitting complaints.
Another FOI reveals more. Peter White was one of the co-lead investigators of the PACE trial. His institution, Queen Mary University of London, received 35 FOI requests over the course of four years. Despite this being less than one request a month they “cannot see an end to these requests”.24
White asserted that the requests were “not in the public interest” and were part of a campaign to “discredit the trial”.
Additionally, “the effect of these requests has been that the team involved in the PACE trial, and in particular the professor involved, now feel harassed and believe that the requests are vexatious in nature.”
What they felt and believed may have been sincere but we have managed to move remarkably far away from accusations of terrorism to what amounts to them not enjoying scrutiny of their work.
Meanwhile, just to keep everyone on their toes, there are multiple people on record claiming intimidation and/or general spite from the PACE researchers and associated doctors25.
For example:
Jonathan Edwards, Emeritus Professor of Connective Tissue Medicine at University College London, who said, "If you criticize PACE in the UK, there is a quiet phone call to your employer and the next morning you are asked to a meeting to reconsider your contract. I get emails from people to whom this has happened. The only reason why I am the only UK academic to call out on PACE is that I am retired so do not have an employer.”
British GP Dr Emma Reinhold explained "I tweeted that I hoped PACE would be discredited and tagged Ben Goldacre, not knowing his connection with Simon Wessely. Within 3 days Simon Wessely followed me on Twitter. His wife sent me a Facebook friend request and the Royal College Of General Physicians said they had received 'complaints' and were considering cancelling the EDS Spotlight project which I had just been appointed to run…”
Dr Keith Geraghty, an Associate Fellow of the British Psychological Society, said that after he published articles “critical of the PACE trial, two of the PACE authors, White and Sharpe, lodged complaints about me and my work to my host University. Emails and phone calls to one’s bosses is very intimidating."
A further complaint which accused him of behaving in an unprofessional manner was made to his home institution, the University of Manchester, by Professor White within weeks of Geraghty requesting access to PACE trial data.
Additionally, the Countess of Mar wrote an open letter to Wessely in which she said that, all the way back in 1998, she had been harassed by him. At that time, she had refused to meet up with him after he wrongly thought she had criticised his work on Gulf War Syndrome. She said she “received a number of telephone calls and letters, both to my office and my home, demanding that I meet you. I have to say that I regarded this as harassment at the time, though I did not see the need to contact the police.”
Eventually she did agree to meet him.26
One of the PACE doctors would also unsuccessfully attempt to get an article by science writer Julie Rehmeyer retracted.
In that article she explained that,
“The study’s defenders painted critics as unhinged crusaders who were impeding progress for the estimated 30 million ME/CFS patients around the world”. 27
Even The Lancet editor, Richard Horton (he who oversaw the recent, controversial, “Bodies With Vaginas” Lancet front cover) pitched in to describe the trial’s critics as “a fairly small, but highly organised, very vocal and very damaging group of individuals” who had “hijacked this agenda and distorted the debate so that it actually harms the overwhelming majority of patients.”
Julie Rehmeyer continued in her article, “Press reports also alleged that ME/CFS researchers had received death threats, and they lumped the PACE critics in with the purported crazies.”
This last thing was quite the neat trick when you think about it.
THE INFORMATION TRIBUNAL
The wheels of bureaucracy thankfully turned and a member of the public, Mr.Matthees, a severe M.E sufferer who lives in Australia, helped achieve the release of the anonymised PACE data.
Queen Mary University of London (QMUL) had refused his initial request, through the U.K’s Freedom of Information Act. They stated fears, “that “motivated intruders” such as ME campaigners or journalists would break the anonymization and publish participants’ names or subject them to harassment.”
He requested an internal review which was also refused and, finally, made a complaint to the Information Commissioner in 2014, ten days before Christmas.
The document that comes out of the 2016 tribunal may reveal the ultimate purpose behind the incendiary narrative of dangerous patients targeting researchers; as a way to obstruct the data of a shoddy, poorly conceived and badly executed trial from ever seeing the light of day.28
The tribunal was less willing to state such a stark conclusion. While acknowledging the evidence before them was not clear they pointed out, more gently, that “if QMUL are cherry-picking who analyses their data from within the recognised scientific research sphere to only sympathetic researchers, there could be legitimate concerns that they wish to suppress criticism and proper scrutiny of their trial”.
Trudie Chalder, a Professor of Cognitive Behavioural Psychotherapy and one of the principal investigators of the PACE trial, admitted through her evidence to the tribunal that there had been no threats to researchers.
She, “accepts that unpleasant things have been said to and about PACE researchers only, but that no threats have been made to either researchers or participants. The highest she could put it was that some participants stated they had been made to feel “uncomfortable” as a result of their contact with and treatment from her, not because of their participation in the trial per se…”
Professor Ross Anderson, one of QMUL’s witnesses, offered the most emotive defence of the deranged activist narrative but the Commissioner gave his input short shrift.
“Professor Anderson’s “wild speculations” about the possibility of “young men, borderline sociopathic or psychopathic” attaching themselves to the PACE trial criticism “do him no credit”. Nor do his extrapolations from benign Twitter requests for information to an “organised campaign” from an “adversarial group” show that he has maintained the necessary objectivity and accuracy that he is required to maintain.”
12,000 people including patients, researchers, journalists and academics had by this point signed a petition calling for the data to be released.
Thankfully, they got their wish.
The last word on the PACE trial should go to Ron Davis, director of the Stanford Genome Technology Center, who said simply, “this is a bad study”.
“The study needs to be retracted,” he added. “I would like to use it as a teaching tool, to have medical students read it and ask them, ‘How many things can you find wrong with this study?’”
As you can tell this area of medicine is characterised by chaos. It is characterised, too, by the contempt with which patients have been treated. So many have been disbelieved, ridiculed and harmed. When I think of those I know with this illness, of how strong and compassionate they are, I just cannot fathom the level of inhumanity.
There are far too many sneering remarks about M.E patients, on the record, to quote, but one made by PACE author and psychiatrist Michael Sharpe, back in 1999, tells us something. He infamously said, “Those who cannot be fitted into a scheme of objective bodily illness yet refuse to be placed into and accept the stigma of mental illness remain the undeserving sick of our society and our health service”.
This seems the source of all venom towards patients. Our refusal to accept the misguided idea that psychiatry is the discipline to help us means we are reviled.
It is sometimes hard to credit that it is doctors behaving like this. Yet the Gender Wars make it clear authority does not mean integrity.
Wessely, at least, has retired from M.E research but it remains to be seen how distant he really is from the field. As well as how long the damage done by the poor science of his ideas will last. His work informs the efforts and beliefs of numerous other doctors and has made its way into popular culture. It has also gone international.
The American-Canadian historian Edward Shorter, for example, not only cited Wessely multiple times in his work but quoted him, too. Meanwhile, the popular 1997 book “Hystories” by American literary critic Elaine Showalter is still helping to push the narrative that M.E is a form of hysteria. Just over half a century since McEvedy and Beard floated the idea. Wessely was reportedly her London mentor. His work was used to make her case, even as she failed to cite more knowledgeable sources or engage with the refutations to his work already in the literature.29
His cruelty to patients seemed to be catching with both of them variously on record being rather sneering. Showalter, at least, added a flair of creativity to her derision, saying of the British term for the disease, “The acronym ME also ironically emphasizes the patient's self-absorption”.
In fact-checking what I knew from memory, for this piece, I came across a very different kind of writing from America. It was a preface written by Mary Dimmock in a document called “Thirty Years of Disdain” which detailed the mishandling of M.E by authorities there. The document’s co-author was her son Matthew Lazell-Fairman who developed M.E at nineteen. I thought her eloquent words should be included:
“I have watched, helpless and heartbroken, as this disease has ripped his life to shreds, turning the promise of a vibrant and spirited future into a soul-crushing existence, at times so unrelentingly harsh and circumscribed, so brutal, so cornered, and with so little hope that I have wondered how he has managed to keep going.
Compounding the heartbreak, it has been disturbing to watch as the world around my son, including his own doctors, has not only dismissed his disease but also ridiculed him for believing that it is real and serious. Worst of all has been the realization that my son is paying this terrible price because the U.S. government has so badly mismanaged the ME crisis since before he was even born.”
LONG COVID
Since the advent of Long Covid, there’s been speculation about whether or not it is the same disease as M.E, or if it is something distinct. A subset of LC patients do go on to meet the diagnostic criteria for M.E.
Early on in the pandemic many M.E patients were noticing some shared symptoms, and worrying about so many other people having to deal with the horrors we know too well.
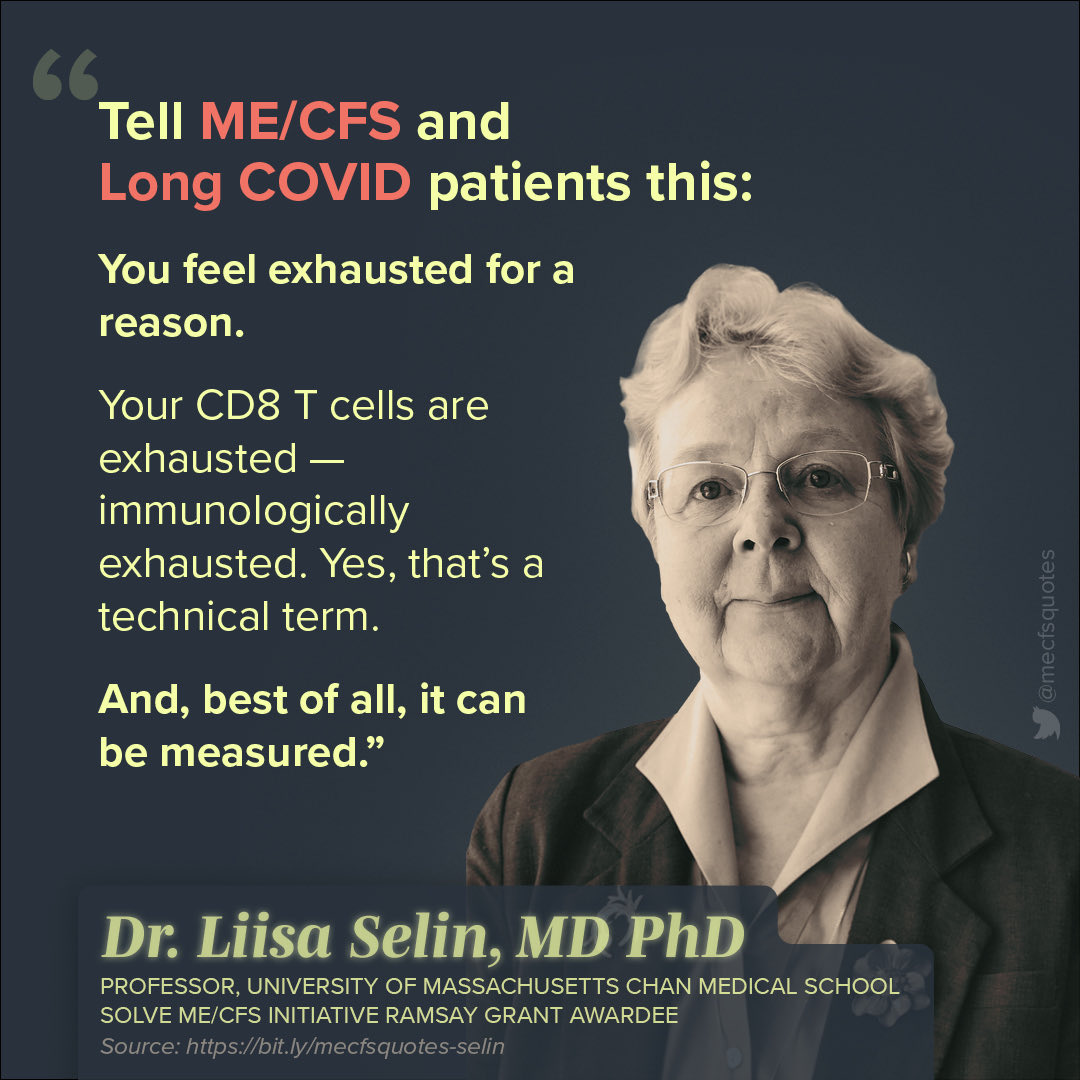
Doctors take differing views on this. Dr. Liisa Selin, a viral immunologist and professor at UMass Chan Medical School, Massachusetts, has been living with M.E for 47 years. Often, she experiments on herself to find answers and has described the severe episodes of M.E she has experienced by saying, “I do feel like I've come back, basically, from being dead each time.”
This is a description many of us can relate to as Severe M.E has long been called “a living death” by those who have experienced it.
On the subject of the similarities between Long Covid and M.E she says
“They are the same disease — or very, very similar”.
“What motivates me to keep going is that I think I know the answer now,” she adds “And I really sincerely do not want other people to have the life I've had. If there's anything I can do to change that, I am determined to do it.” 30
Her resolute desire to help people is encouraging.
Dr. Maureen Hanson, Director at the Centre for Enervating Neuroimmune Disease and a Professor of Molecular Biology and Genetics at Cornell, is more circumspect about whether the two illnesses are identical. She cautions against concluding that common symptoms must mean the same underlying mechanism. As well as noting the importance of continuing specific M.E research. Something less likely to happen if we simply assume they are the same before we prove it.
All the time such thoughtful minds are focused on these illnesses, the outcomes for those who are suffering stand to be promising.
There is the risk that the politics of Long Covid will become mired in the same troubles we have seen affect M.E patients, though.
Familiar bad actors are likely to take advantage of this additional avenue of money and potential acclaim, when and where they can. Wessely, for one, seems keen to share his “expertise” at the drop of even the merest hat. PACE author Michael Sharpe, for another, is already evident on the scene.
In a talk called “Post Covid 19 syndrome (Long Covid)” at Zurich insurance company SwissRe he referenced the PACE trial as though it isn’t utter hokum. He then went on to state, without any evidence, that “at present the best treatment is psychologically informed rehabilitation” (for Long Covid patients). 31
Companies and governments who are unwilling to face the expenditure of caring for a large population of seriously ill people, especially seriously ill women, may be grateful to doctors like Sharpe.
In order to get away with that, however, they’ll need enough of us general rabble to be willing to believe them. They will need us to accept that patients are to blame for failing to recover because they are lazy or neurotic or hysterical , and to help propagate that idea.
We don’t have to allow this to happen to a group of people, again.
FINAL THOUGHTS
Lately, M.E has been getting mentioned more in the online circles many of us share. As a lot of you may not have heard of it before, I thought you would be interested in this history. Especially those of you who are feminists or who are concerned with medical ethics.
A lot of M.E patients will disagree with the position I take on gender politics, but I know a notable number of the women raising concerns about ethics in gender medicine have M.E. We turned up for this fight precisely because we have been at the centre of our own medical scandal. What is being done to dysphoric children, by the medical profession, chimed a bell within us. Especially those of us who were children when we became sick. The harms are different but the sense of needless cruelty is the same.
We are also well aware that what people say about a group is not always true, or fair.
So when we saw women who spoke up threatened as “terfs” we asked questions and sought out information instead of merely believing in your villainy. Something that led to us being called “terfs” ourselves.
We are gladly amongst those women fighting beside you now. We are often the women quietly doing work, behind the scenes, while unable to join your gatherings. We may not have hugged as many of you as we want to or stood beside you on the physical front lines but we are here.
Inevitably, when conversations about M.E crop up there will be people pushing pseudoscience because they have been misinformed, or because they wish to misinform. Most of the time that blends into the background for a group of people who have had to become used to being misrepresented. It is always harder, though, if it comes from people we like or admire.
I have never lost the slight sinking feeling that comes with telling people what illness I have. Or the moment of waiting afterwards to see if the person I care about is going to respond with decency, or something more disappointing. In that sense, such a diagnosis is a social litmus test. Does someone accept a popular, derisive narrative about a group of ill people, especially when they are mainly women, or do they ask questions?
Many of you will relate to this; how people respond when you articulate your sincere, yet heretical, views about Self-ID is a social litmus test as well.
The truth so often does need time to get its boots on. This is why the same spirit of enquiry and willingness to dissent that has brought you into discussions of women’s rights, and the fight against a harmful ideology, is needed on the subject of M.E, also.
For both communities having a particular cause as a rallying point neither defines us as people or proves to be all we have in common.
When it comes to the M.E community our defining feature as a group is not illness, after all. It is tenacity.
https://publications.parliament.uk/pa/cm200607/cmselect/cmhealth/503/503we79.htm


I am in awe, thank you for articulating so clearly how people, mainly women have been treated with such callousness by Dr's who swear to "do no harm".
Anyone reading this (imho it should be mandatory) can see the medical, political & media organisations have catagorically failed each & every single ME/CFS patient!
My heart aches for you & all chronically ill people, no one chooses to be ill, s/t we have no choice.
May 2020 I was DX'd with decompensated Cirrhosis & given 2 days to live. So thankful to the SNHS.
10 yrs previous to this I was DX'd with Adult ADHD, Fibromyalgia, kidney stones & Ulner nerve entrapment syndrome.
I was told (quite glibly) I had Non Alcoholic Fatty Liver Disease.
At the same time I was questioning the amount of fatigue, pain, weight gain, bone pain, joint pain I was experiencing.I turned to the Web, looked up my symptoms, luckily my GP's believed me, it took a Yr eventually I was DX'd with Hyperparathyoidism. After that I've had 2 TIA's, Acute Appendicitis, & DX'd with Diabetes T2 & given birth to approx 40 kidney stones, lost all of my teeth & I look like I'm pregnant with an elephant (Diastasis Recti) which cannot be fixed b/c of the cirrhosis.
Yes, back to the cirrhosis, even after 2+yrs I still can't process it, my sister kindly pointed out "one of the first things people are going to think is that you are an alcoholic", a couple of weeks ago my GP said the same. I don't drink! In my instance it it excess fat accumulating in the Liver (highly likely to be hereditary). I am angry! Only recently I was told that the NAFLD & the type 2 diabetes had accelerated the damage to the liver, it usually takes 30 odd yrs from NAFLD to cirrhosis, mine took 3 yrs!
WHY did no one mention this when I was first dx with NAFLD, my only cure is transplantation or death!
I feel I have to explain/give a reason or defend myself as to why I look very heavily pregnant (Acites) at 56!
Like yourself I do wonder every day if I will ever feel well enough to join society for any length of time again.
I so hope you can at least enjoy some good times.
Please take very good care of yourself, you deserve to have a good life, just like those who are lucky enough not to be *blessed*(sorry, my sense of humour, comes from having 2 sons with ADHD, S.I.D, Dyspraxia & ASD. Fighting to get their needs diagnosed took 10yrs & threats of losing them, that's another story to tell!)
Much love and gentle hugs 🤗
P.S I agree with you about Self I.D, There are going to be some really messed up young minds in the very near future.
All in the name of money!
On a very quick skim, a very thorough and comprehensive description of a medical condition I hadn't been aware of. Of course many people wind up with the short end of the stick in life's genetic lottery, but M.E. seems one of the worst outcomes.
Interesting though that the sufferers of those conditions are often the activists who are the impetus for changes for the better. Reminds me of having seen Lorenzo's Oil several decades ago:
"Lorenzo's Oil is a 1992 American drama film directed and co-written by George Miller. It is based on the true story of Augusto and Michaela Odone, parents who search for a cure for their son Lorenzo's adrenoleukodystrophy (ALD), leading to the development of Lorenzo's oil."
https://en.wikipedia.org/wiki/Lorenzo%27s_Oil